




Dr Rodney Syme is to be applauded for his courageous act in ''outing'' himself as the person who supplied my brother with the Nembutal that allowed him to end his life painlessly, with dignity, and at a time of his choosing (Focus, 28/4). Palliative care was not for Steve. He was fiercely independent and hated the idea that others might take control of the last few weeks or days of his life, regardless of how caring they might be. The change in Steve after he had been supplied with Nembutal, and he knew he was in control, was profound. Until then he was depressed and angry, but afterwards he became more cheerful and calmly accepting of his situation. Voluntary euthanasia has been ignored by politicians for too long, and Dr Syme has taken his brave step to force them to tackle the issue.
Andrew Guest, Balwyn NorthI am 100 per cent behind you, Dr Syme. I have terminal oesophageal cancer and am making the most of my time - possibly another six months - surrounded by family, friends, a great set of doctors and a palliative care team. My instruction to all is I don't want pain, I don't want to be in a hospital and I don't want to live longer than necessary when the time comes. Who would argue? But this is where our legislators ignore us. How do I ensure my wishes and needs will be met? I can stockpile barbiturates and overdose (not a good role model as a father of a 22-year-old son or to the wider community); search for a Dr Syme; or trust a broken process. Let us all unite behind Dr Syme to drive fundamental change.
Peter Short, CamberwellWe all cling to the stories like that of my grandfather, who went to the bowling club, had a beer with friends and died of a massive heart attack as he put down his first bowl. He was 80 years old. It's the sort of end we all want to believe will happen to us. The truth is very often far different. It involves pain, poo, fear and indignity, and almost inevitably a feeling of helplessness. Watching my father die of cancer in this way made me know that choice is the key. I make choices every day. One day, for medical reasons, I may make the choice to end my life - always supposing that bowls doesn't get me first.
Perhaps selfless doctors like Rodney Syme will make it possible for me to make this choice calmly, rationally and in my own time. The alternative is messy, lonely and a horror for my family.
Sally Dobson, South MelbourneI wholeheartedly support Dr Syme's campaign. I'm in the last quarter of my life and, facing the inevitability of my mortality, I find myself filled with fear. Not a fear of dying, but of being consigned to a nursing home where I'll end my life in loneliness, being fed and washed by overworked staff, with no family in this country to visit me (a common plight of migrants and those who have not had children). Why, oh why, can't we allow people to decline to be kept alive? And if they need a doctor's assistance, then the physician should have the full authority of the law to render it.
Patricia Summers, CanterburyDying with dignity via assisted suicide happens - every day. Surveys of doctors consistently show they assist the terminally ill to die, and families with means provide the help to their loved ones. The lack of prosecution reflects society's recognition that this is compassionate assistance, supporting the choice of the dying person, and not a criminal act. The law urgently needs to catch up with current social values.
Janine Truter, The BasinRodney Syme has campaigned for years to achieve what politicians nationwide have for generations been unwilling to provide - a legal mechanism that would allow us to die with dignity at a time of our choosing when no other option is viable. Now Dr Syme has put his own welfare on the line by challenging the authorities to try him in open court for assisting someone to die.
Dr Syme has no need to challenge the law for his benefit because he already has access to the drugs necessary to achieve a peaceful end. Instead, he is acting on behalf of the huge majority who have waited in vain for leadership, and have been denied a right to a peaceful death by generations of reluctant politicians.
All Australians should lobby their elected representatives to take positive and compassionate action to end the needless suffering of all those who are forced to die badly. Without such laws, self-deliverance can only be achieved crudely, separated from family and friends. Rather than prosecuting a man of principle, we should be changing archaic laws.
Bob Thomas, Blackburn SouthIn his act of compassion, Dr Syme merely provided Steve Guest with assistance that the state should be making available to all citizens who want to take control of their deaths when in similar circumstances. Three US states now have dying with dignity legislation and the sky has not fallen. In Oregon (population approaching 4 million) last year 122 people were provided with life-ending medication and only 71 used it - supporting Dr Syme's theory that possession of the means is palliative. The published photo of Steve Guest showed him as a young healthy man; an image of him in those last dreadful weeks might have been too horrific for publication.
Anne Riddell, Mount Martha
Editorial in The Age:
Nine years ago, 58-year-old Steve Guest was dying from oesophageal cancer, and in intolerable physical and psychological pain. In July 2005, he took his own life with an overdose of a barbiturate used by veterinarians to kill animals. What has not been known until this week is that Mr Guest was supplied with this lethal drug by Dr Rodney Syme, a Melbourne urologist and campaigner for voluntary euthanasia, who had visited the terminally-ill man at his Point Lonsdale home in the weeks before his death. We know this because Dr Syme himself told The Age on Monday that he had done so.
Dr Syme, the vice-president of Dying with Dignity Victoria, said he had not chosen to speak out until now because he had not wanted to face the stress of a possible trial or conviction. Inciting, aiding or abetting a suicide is a criminal offence in Victoria and carries a maximum penalty of five years' jail. As we reported yesterday, Victoria Police has reopened the investigation into Mr Guest's death.
Dr Syme changed his mind, he told The Age's health editor Julia Medew, because he believes that creating a court challenge could set a useful legal precedent and accelerate the public debate on euthanasia. ''I just believe passionately that there are too many people suffering too much not to try a little bit harder to change things,'' Dr Syme said.
He draws a useful parallel with abortion reform in Victoria - another example of a once illegal practice that was partially decriminalised in a court case in which a judge ruled it to be reasonable. This effectively brought an end to a climate of secrecy and corruption similarly echoed by the present black market in this country for the drug Mr Guest took.
Certainly, as Dr Syme well knows, there has been woefully little progress in public discussion on all aspects of rational and assisted suicide. In fact, in political terms, the matter has sunk into inertia. Over the past 20 years, state Parliament has rejected 16 euthanasia bills, and Victorian Attorney-General Robert Clark said this week the government would not explore such legislation; nor would it refer the matter to the Victorian Law Reform Commission. This has provoked Dr Syme into taking such risky action. He is a courageous man.
The Age is committed to the encouragement of community debate on euthanasia because we believe it is only through such full and informed means can there be wider understanding and acceptance. However, we remain concerned that changing the laws on voluntary euthanasia and assisted suicide could result in possible ambiguities or abuses: euthanasia, as we have said, should not be permitted to become a subtle form of murder. Care and consideration are therefore essential.
What is clear, though, is that the public mood on rational and assisted suicide has changed, and has become more accepting. Part of this could be ascribed to specific examples. A year ago, The Age reported the remarkable story of 83-year-old Brighton woman Beverley Broadbent, who, before ending her own life, told us that she was ready to die. More recently, we reported on how 78-year-old advanced-dementia sufferer Sue De Ravin, who, despite writing a ''living will'' that would prevent her being resuscitated, is legally prevented from her death being hastened in any way.
The Victorian Law Reform Commission is, in fact, the ideal forum for community debate on euthanasia. Such a group of independent experts are ideally placed to receive submissions and report back in detail. The Napthine government should quickly overcome its reservations to refer the matter to the commission. Society expects nothing less.

Letters in The Age:
If Victorians decide to legalise physician-assisted suicide, one hopes it will be based on careful debate and not on sensationalised declarations of need from a minority of doctors. The community might then better understand why the majority of doctors continue to oppose legalisation. This is based on factors including the rarity of requests from patients receiving good palliative care, the possibility that requests are driven by distressed relatives, the difficulty in drawing up laws that adequately protect vulnerable people who feel they are a burden to society, and the undermining of trust in doctors generally if some participate in physician-assisted suicide.
Should legalisation become a reality, that assistance should be provided by persons other than doctors, or by a small number of clearly identified doctors, so that trust in doctors generally is not undermined. Involving doctors seeks to legitimise as a medical process what is really a social and legal intervention.
Dr Kerry Breen, KewIt seems Rodney Syme is not going to get what he wants and indeed might get what he doesn't want - a prison sentence. Why is it that on 16 occasions state parliaments have knocked back what 80 per cent of Australians for decades have declared they want - the legal freedom to determine the manner and timing of their death in the circumstance of a distressing and incurable terminal illness?
Has this 80 per cent not been hammering on parliament doors loud enough? Or is it that powerful and well-funded lobby groups from medicine and religion are pounding harder? Or do our politicians only listen to the community on selected issues?
Kenneth Ralph, Belmont
Letter in The Age:
Dr Kerry Breen (Letters, 30/4) says, ''the majority of doctors continue to oppose legislation'' on physician-assisted suicide. As a practising GP in favour of legislation on physician-assisted suicide, I wonder where the evidence for this statement comes from? As far as I am aware, there is a dearth of it on current attitudes of Australian doctors to dying with dignity legislation. Recent surveys show that most of the general population support this type of legislation. I am not asking Dr Breen to assist anyone in their end of life, but only to not oppose a law that allows this to occur legally. A law I hope allows me the opportunity to use it, if the need arises, at my end of life.
Dr Simon Benson, Footscray
Article in the Sunday Age:
Voluntary euthanasia is an issue that just won't, well, die. Why is it an issue of such persistent public debate - and what might resolve it one way or the other? Julie Medew takes the pulse of a divisive debate:
1. Dying with dignity - it’s an unresolved debate that returns periodically to haunt the political cycle. Are those in favour and those opposed so fixed in their positions that the problem is intractable?Many polls have consistently shown about 70-80 per cent of Australians believe a doctor should be able to provide a dying person with a lethal drug to end unrelievable suffering at the end of their life. This support has been noted by more than a dozen politicians who have proposed laws in every state parliament except Queensland over the past 20 years. But most of these attempts have failed due to a lack of support from other politicians who are usually asked to vote on their conscience. A lack of majority support from politicians has been the main barrier to law change, except in the Northern Territory which legalised voluntary euthanasia in 1996. The law only lasted nine months though before the federal government overturned it.
2. If the overwhelming majority of Australians are in favour of voluntary euthanasia why are so many politicians against it?Very little research has been done into the motivations and perspectives of politicians on voluntary euthanasia and physician-assisted suicide, but one study did examine how federal politicians voted in a conscience vote to overturn the NT’s euthanasia legislation. It found three key factors at play: party alliances, gender differences and, most of all, religious affiliation. All Catholic politicians and all but one from other Christian denominations voted to repeal the NT law. Last year all Liberal MPs voted against a bill in Tasmania, compared to 7/10 Labor members, causing speculation the Liberal MPs had resolved to vote along party lines rather than on conscience.
3. What are the main arguments in favour of voluntary euthanasia laws and who are the main champions?Many civil libertarians, some doctors and organisations such as Exit International and Dying with Dignity argue that palliative care does not always alleviate suffering, especially existential and psychological distress at the end of life. They also say that a fundamental principle of a liberal democracy is the right to self determination, so if a competent person understands their diagnosis, prognosis and treatment options, and wants to choose the way in which they die, they should be allowed. Another argument is that, because doctors already are helping people die in an unregulated fashion, legalisation would ensure appropriate safeguards and oversight.
4. What are the main arguments against changing the laws and who are the main players here?Many religious groups, doctors and ethicists argue that human life is paramount and that decisions about life and death should be reserved for "divine agency". While all legislation has proposed safeguards, opponents say it is impossible to guarantee a person is asking to die completely voluntarily. They say people approaching the end of their life, particularly the elderly and disabled who are relying heavily on others for care, may feel subtle pressure to stop burdening others and end their life. There also is a fear of the ‘‘slippery slope’’ eventually allowing euthanasia for children, people with psychiatric illnesses or in non-voluntary circumstances where people are not able to express their view at the time of a decision.
5. Last week Melbourne doctor Rodney Syme went public with his assistance of a terminally ill patient to end his own life nine years ago - a move that he says is designed to test the law. Is he mad, bad, or just dangerous to know?Dr Syme says he has helped hundreds of people die since he had an epiphany 38 years ago while caring for a woman dying in extreme pain with kidney cancer, for whom nothing more could be done. Since then the urologist and vice-president of Dying with Dignity Victoria has been giving terminally ill people the knowledge and means to end intolerable physical and existential pain that he believes cannot be relieved in other ways. He says it would be unconscionable not to help people in such circumstances and that he does not assist people with psychiatric illnesses to end their own lives. His phone number is hot property among people who believe in assisted dying and want help.
6. How might Dr Syme's move play out?Victorian police have started investigating Dr Syme’s admission. If they charge him with possessing an illegal substance and/or inciting, aiding or abetting a suicide, it could result in a court case. The maximum penalty for assisting a suicide is five years’ jail. If Dr Syme is found guilty and jailed it will send a clear message to doctors that what he is doing is illegal. If he is found not guilty the court ruling could set a powerful precedent for doctors who want to help people die in similar circumstances but are too afraid of the law to do so. If he is not charged some may argue the law banning assisted suicide is useless and should be scrapped.
7. Could a test case like this lead to a new law in Victoria?Dr Syme says the unregulated and covert practice of assisting people to die reminds him of the clandestine abortions carried out in Victoria before the ‘‘Menhennit Ruling’’ in 1969. During the trial of a doctor accused of illegally performing an abortion, Justice Menhennit ruled that terminations can be lawful if necessary to protect the physical or mental health of a woman. The judgment effectively allowed abortions to be performed in some circumstances and paved the way for a conscience vote in 2008 which decriminalised abortion in Victoria.
8. Has legal change permitting voluntary euthanasia had unforseen consequences elsewhere?Anti-euthanasia campaigners say the "slippery slope" argument has played out in Belgium, which this year became the first country to allow euthanasia for terminally ill children of any age. Under the law, children seeking to die must be "capable of discernment" and psychologists must confirm they understand what they are doing. Parents also must approve of their child's decision. In the past 18 months Belgium also controversially allowed euthanasia for deaf twins who were about to go blind and for a transgender person who wanted to die after an unsuccessful sex-change.
9. How can society be confident sick people wanting to die are acting of their own free will and are of sound mind?It all comes down to the safeguards built into the law. In the most recent Tasmanian bill a patient asking their GP for help to die would have had a three-day cooling off period, during which their GP could consider the case for alternatives to death. If the patient was assessed as competent and reasonable, their request must be put in writing and witnessed by two other people, only one of whom can be family. A second doctor must then agree that the person is suffering intolerably from an incurable condition, and that there are no alternative treatments. After a week a fatal drug then could be administered. The request could be rescinded at any time, and no-one would be compelled to be part of the process.

Article in The Age:
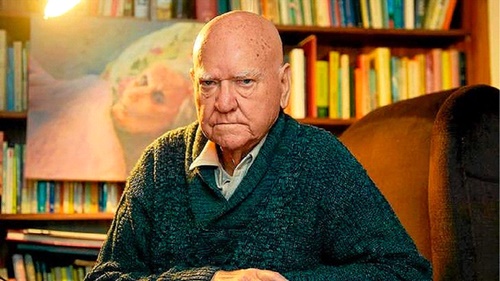
Doctor Percy Rogers admits he helped someone die. Photo: Joe Armao
Another Australian doctor has admitted giving a man a lethal dose of a drug at the end of his life and has spoken up in a bid to highlight the need for a debate about voluntary euthanasia.
One week after Melbourne urologist Rodney Syme dared police to charge him over his provision of a fatal drug to a dying man, Dr Percy Rogers said he had also helped a terminally ill man die.
Dr Rogers, a locum GP, said about 47 years ago, he got a call to attend to a friend of his who was clearly suffering as he approached the end of his life with lung cancer.
"He was on the bed gasping in terrible pain and was looking for some relief from the pain, so I ordered 20 milligrams of morphine ... A nun who had accompanied me there said 'But doctor, that will shorten ... ' and then stopped; she said no more. What I’m sure she was going to say was 'that will shorten his life'.
"That was about 11 o’clock at night and then I had a ring in the early hours of the morning to say he had passed away. I’m certain that it [the morphine] depressed his respiration and shortened his life. It shortened it probably by a matter of hours rather than days."
Dr Rogers said although the dose was capable of hastening his friend's death, his primary intention was to relieve his pain.
"He was in considerable distress and my training as a doctor was to relieve people’s distress ... I felt I was doing my job," he said.
Dr Rogers chose to speak out about the death, which he said could arguably be labelled euthanasia, to support Dr Syme, the vice-president of Dying with Dignity Victoria.
Dr Syme last week admitted he had given Steve Guest, a 58-year-old-man who was dying of oesophageal cancer, a lethal drug which he used to end his own life in 2005. Police are now investigating the admission. If Dr Syme could be jailed for up to five years if charged with inciting, aiding or abetting suicide.
Dr Rogers said he had also given terminally ill people prescriptions for lethal amounts of drugs on rare occasions in the past after being assured they were of sound mind and would not use the drug "lightly or mischievously". He said he did not know if they ended up using a fatal dose of the drug or not.
"I think there must be a community debate about this ... The population is ageing, so this is going to be a problem confronting a lot more people," said the GP, who works regularly with indigenous Australians in remote communities.
Dr Rogers’ disclosures came as the group Doctors for Voluntary Euthanasia Choice said they supported Dr Syme and wanted voluntary euthanasia to be legalised for terminally ill patients with intolerable symptoms. The group of almost 100 doctors, including GPs, surgeons and specialists from around Australia, said end-of-life assistance "should be a final, compassionate act of palliative care and should be legal".
A spokesman for the group and retired Adelaide gynaecologist and obstetrician, Arnold Gillespie, said he believed other doctors were taking similar action to Dr Syme and helping terminally ill patients suffering incurable pain to end their lives.
"Undoubtedly there are doctors doing that out of compassion for their patients when the medical profession has nothing else to offer," he said.
Associate Professor Gillespie said in his career as a gynaecologist he had been confronted with patients "in the terminal phase of ovarian cancer for whom relief could not be obtained".
He said various polls had shown overwhelming community support for voluntary euthanasia for patients experiencing unrelievable and incurable suffering, and it was time for politicians to reflect community attitudes by legislating in favour of it.

Letter in The Age:
We write in support of Dr Rodney Syme who has admitted his part in the death of Steve Guest in 2005. Steve Guest died by his own hand, using a drug supplied by Dr Syme. The police decided that no action was required but now are likely to investigate, given further information supplied by Dr Syme. Given the failure of legislatures to enact permissive legislation, Dr Syme has concluded that a favourable judicial conclusion may influence the Parliament to take action.
We write also to contradict the ill-informed belief that doctors are opposed to liberalisation of the law. We strongly support the modification of the law to permit voluntary euthanasia and physician-assisted dying in legally defined circumstances.
We favour a legal framework in which decisions to end life are entirely patient-centred and not reliant on the views of a doctor. We are appalled that currently it is illegal for doctors to even sit with a terminally ill person with intolerable symptoms, who has decided to take his or her own life. End-of-life assistance in whatever form should be a final, compassionate act of palliative care and should be legal.
Professor Tony Adams and 98 supporters
Editorial in The Age:
Significant social change has always needed the courage of a few. The suffragettes, literally, put their bodies on the line to win voting rights for women; Emily Davison famously stepped in front of King George V's horse at the 1913 Epsom Derby, suffering injuries that caused her death four days later. Students protesting against the Vietnam War at Kent State University in 1970 faced the guns of the Ohio National Guard. Four were killed.
Those advocating additional rights for women, such as abortion, or seeking the recognition of Aborigines, gays, and now same-sex marriage have all faced abuse, vilification and, at times, the threat and actuality of violence.
Too often they gain the support of the majority yet must persist with their fight because their representatives in Parliament take far longer before accepting that the law does need to change to reflect the community's views.
The issue of same-sex marriage is, arguably, today's leading social dispute. We have seen lawmakers in the Australian Capital Territory understand society's changed view, only to be thwarted by the High Court at the behest of the federal government. The law will eventually change, it is simply a question of when.
That issue, however, will quickly be overtaken by that of voluntary euthanasia. It will be a divisive and emotional debate, but our changing demographics, whereby those aged over 65 are projected to double to 25 per cent of the nation's population, will demand it be confronted.
A leading advocate has, for many years, been Dr Philip Nitschke. There is no question he has been a polarising figure, with an overt campaign that has pushed the boundaries of legal and community acceptance. Ground-breakers test the limits; some of Britain's suffragettes were widely criticised for their militant tactics, which included arson and assaulting police.
The momentum for a broad community debate on voluntary euthanasia is building, as individuals tell their stories about why they would wish to take control of their own death, and the medical profession explains the realities of treating such patients.
In the past week, of course, Dr Rodney Syme has shown remarkable courage in explaining his role in the death of cancer sufferer Steve Guest, to the point where he has identified the drug he used. Dr Syme has, in effect, defied the prosecutorial authorities to charge him with a criminal offence, so that he can make his case to a jury and seek their wisdom as representatives of the broader community.
In Thursday's Age, he was joined by Dr Percy Rogers, who for the first time explained his role in the death of a friend nearly half a century ago. His admission, that he used morphine to help his friend die, may also place him at legal risk. Our letters page, too, featured one in support of Dr Syme from 99 members of the medical fraternity from around the country. Its lead signatory, Professor Tony Adams, made the point that it is illegal for doctors to even sit with a terminally ill person, with intolerable symptoms, who has decided to take his or her own life.
Professor Adams and the other signatories emphasised that doctors strongly support a change to the law, to allow voluntary euthanasia and physician-assisted dying in legally defined circumstances. The Age agrees, and reiterates our belief that the Victorian Law Reform Commission should be the forum to enable this vital community debate to reach sensible legal proposals that can then be adopted by Parliament. It should not take a trial of a respected medical specialist to prompt this obvious progression. History has enough martyrs.

Letters in The Age:
I applaud Dr Percy Rogers in his telling of how he relieved his friend of a miserable death by doses of morphine (''He was on the bed gasping in terrible pain and looking for some relief'', 8/5). Dr Rogers is a member of our medical group supporting legislation to permit legal voluntary euthanasia. He is one of about 100 doctors who are able to proclaim publicly that they stand in favour of voluntary euthanasia. I, too, recall clearly how many years ago as a young locum specialist in England, I came across this sad individual lying near death in a side ward. She had had ovarian cancer that her doctors had missed and I surmise they felt too guilty to let her go. I instructed the nursing sister to give large doses of morphine and by the following morning the poor woman was dead, much to everyone's relief. There are so many of us doctors performing this illegal act that it is almost conventional and dare I say, ''best practice''. I wish Rodney Syme every success in his campaign.
Dr Rosemary Jones, North AdelaideWhat if every doctor in Australia who has compassionately acceded to the request of a terminally ill patient to hasten their death now admits it? The weight of that challenge will surely force governments to reform the law and decriminalise the act. Of course, every such case is going to be nuanced, but not so much as to prevent perfectly workable safeguards being devised to prevent abuse. Just as with pregnancy terminations, not every doctor will want to involve themselves in compassionate assisted dying and will have the right to abstain. But won't it be great when we can ask our medical practitioners if they practise it within the law, and thereby choose between them - either because we may want the option for ourselves, or because we most definitely disapprove. The main reason for opposing assisted dying and other end-of-life choices is religious belief. But this cannot be allowed to influence law-making in a modern, secular society where more than 80 per cent of citizens approve of letting the terminally ill choose how and when to die.
Anne Riddell, Mount MarthaHow much longer can our ''representatives'' ignore the wishes of the people that put them in Parliament? Dr Percy Rogers and (at least) 100 other doctors (Letters, 8/5) - who will know what they are talking about far better than the MPs who stand in the way of compassionate legislation for choice - are only underlining what most Australians are asking for: the right to choose when to die if fate deals them a bad hand. Roll on the day when these King Canutes are overwhelmed by the waves of public opinion.
John Millard, East DoncasterProfessor Tony Adams (Letters, 8/5) fails to mention the option of palliative sedation as an alternative to euthanasia. The intention of the former is to relieve suffering, the intention of the latter is to kill the patient. The former requires time and effort in good ongoing nursing and medical care; the latter requires little time or effort. The former is already legally available, the latter would require legal changes with safeguards that cannot deliver. If there are concerns that patient suffering is not being relieved, the answer is surely in better use of what is already available, rather than just killing people.
Geoff Sheahan, Wantirna South
Letter in The Age:
In my 50 years as a doctor I would not have hesitated to act exactly as Dr Percy Rogers reportedly did if presented with the circumstances described. Giving morphine for the purpose of relieving pain even though the unintended consequence of respiratory depression may result has, in my opinion, never been considered unethical let alone illegal. It is good medical practice.
Of much more importance to the debate are two other questions: Does a patient's autonomy, in the absence of a terminal illness, give them the right to demand physician-assisted suicide, as was permitted for a short time in the Northern Territory? And should euthanasia be allowed for patients who cannot give informed consent, such as children and the demented?
Irwin Faris, Torquay
Article in The Age:

Former Victorian speaker Ken Smith has called for a renewed debate on euthanasia - free from "religious fanaticism" within State Parliament - so terminally ill patients would have the right to seek assistance to die. Six years after state MPs voted down proposed "dying with dignity" laws, Mr Smith, a Liberal veteran who co-sponsored the original bill with the Greens, is again pushing for legislative reform.
"I'd like to see the whole issue referred off to the Law Reform Commission, which could come up with an independent opinion on it, not driven by religious fanaticism," he said. "Parliament could then take up the commission’s recommendations."
Mr Smith's comments come after voluntary euthanasia campaigner Dr Rodney Syme admitted giving a dying man the lethal drug Nembutal two weeks before the man killed himself with it at his Point Lonsdale home.
Dr Syme told Fairfax Media last month he had decided to "out’" himself and be charged over the death because a court case could set a useful legal precedent for doctors who are too scared to help terminally ill people end their life. Police are believed to be investigating the matter but have yet to charge him.
Mr Smith described Dr Syme’s actions as a "courageous", and also said his own views on euthanasia were shaped by the deaths of his sister and brother, both of whom died of cancer and had suffered intolerably.
"My sister had cancer right through her body. She was in palliative care, and they took care of her magnificently, but she was in really terrible pain," he said. "My brother was the same - he died of lung cancer and really suffered. There should be legislation in place to allow people who want to die with dignity to be able to do so. It’s not as if legislation would make it compulsory; it would just give people the right."
In Victoria, inciting, aiding or abetting a suicide carries a maximum penalty of five years’ jail. But the issue was a matter of heated debate at Spring Street in 2008, when Greens MP Colleen Hartland introduced the Medical Assistance (Physician Assisted Dying) Bill into the upper house, where it was eventually voted down 25 to 13 in a conscience vote.
"A bunch of religious zealots knocked it out with some of the lies that they told and the scaremongering," said Mr Smith, who declined to identify individual MPs.
He said he felt free to revisit the issue now that he was no longer the speaker, having quit the job and returned to the middle bench earlier this year after a tumultuous term in the chair.

Letters in The Age:
I'm now in my 80s, in the evening of life but still of sound mind, a retired doctor having seen many die, a former Catholic priest having sent many on their way. My view on the right to die at a time of one's own choosing is imposed on no one; on the other hand, the view of those opposed to euthanasia is imposed on everyone - that is the injustice (''Reject euthanasia and save us from Dr Death'', Comment, 12/5).
Dying is a lonely event, eased but not shared by those who love us. The real pain of dying is not the physical pain, which can be easily relieved; it is the pain of irretrievable loss of dignity, of control over one's destiny, bodily functions and independence. It is the pain of fading memories, the pain of waiting with the realisation that one day we will be no more than a name on a family tree. These things can never be relieved by palliative care. My life is my own and I wish for the freedom to die with dignity when I decide, surrounded by those who love me and within the constraints of a law framed to shield me in that dying hour.
Dr Peter Evans, HawthornNicholas Tonti-Filippini has for years campaigned relentlessly against medically assisted suicide. He now suggests that such legislation would be discriminatory because it would allow him an additional choice at the end of his life. How the provision of choices can be viewed as discriminatory defies logic. The very essence of dying with dignity reform revolves around the word ''voluntary'' and is predicated upon choice. He also states that Steve Guest's suicide was unlawful, which it was not as suicide is legal and the decision to choose that option was Mr Guest's.
Experience has shown that where a terminally ill patient has an option to end their life, often this knowledge alone is sufficient to give them the strength to battle their illness a little longer.
Bob Thomas, Blackburn SouthNicholas Tonti-Filippini extols the virtues of palliative care medical staff, while treating people like Dr Rodney Syme as if they are in some way repulsive. His overuse of the term ''Dr Death'' is disrespectful and inaccurate. Tonti-Filippini oils his text with allusion to his own condition, and puts forward an assumption that to live longer is undeniably preferable to ending a life that has become unendurable. What he fails to acknowledge is that doctors like Rodney Syme are not on about the law supporting them to end the lives of people against their will. If such were the case then maybe his allusion to Nazi death squads might have merit. Dr Syme simply wants legislators formally to acknowledge it is possible for an adult who has reached the end of viable life to make an informed choice to end suffering.
George Wills, Mount DandenongIf Nicholas Tonti-Filippini can't make his case without inflammatory language such as ''Dr Death'' then he shouldn't be given a public voice. It is an insult to doctors who care deeply about real people, suffering in the real ''here and now''. He can think what he likes, but let's not allow him to inflict his views on others and make them suffer just because of his religious beliefs.
Rod Andrew, MalmsburyThe last person I would want to see at the end of my bed would be Nicholas Tonti-Filippini suggesting his views on end of life are preferable to mine. I have made my choice and respect the right of others like Tonti-Filippini to follow their beliefs.
Ruth Boschen, Balwyn
Letters in The Age:
My youngest brother Stephen was dying a prolonged and painful death. Only two good things happened to him in his final month: he found through ABC talkback radio that there was huge sympathy for him throughout the state - he wasn't dying alone - and, following this, he had his Nembutal, his ultimate release, his death. The profound difference these two things made to his near-destroyed morale were the only positives in a sea of misery. Nicholas Tonti-Filippini (Comment 12/5), a Catholic ethicist, finds fault with this. He believes Steve should have died properly in bed, on his back, drugged to the eyeballs and having his bum wiped by paid strangers. The very things he did not want. But it was not ''the Steve Guest saga'', or ''a euthanasia cause celebre'': it was the story of how a very brave man coped with his barely tolerable circumstances. The help given by Rodney Syme - both valuable advice and medication - was uplifting for Steve.
The contribution from the religious was negative. Those with Christian love at heart were silent. The crackpots came to his door exhorting him to only have faith and Jesus would welcome him. Others were vicious, like the anonymous writer of a beautifully printed card I found at the house on the day of his funeral, telling him self-murder was the greatest crime and the wages of sin were death. In comparison, the police were splendid - courteous, understanding and sympathetic.
Unlike Tonti-Filippini, I thought at the end of that sad episode that no evil had been done and that a little bit of good had been achieved.
John Guest, CamberwellNicholas Tonti-Filippini speaks for himself but also embodies the agenda of the Catholic institution he works for. He does not speak for me or for all the terminally ill. I, too, have a chronic illness, an incurable neurodegenerative condition that I have watched others suffer and die from. Conditions like mine eventually rob the sufferer of any independence and any shred of dignity; palliative care is largely ineffective.
I have a fulfilling life now, but I know what my future inevitably holds and the greatest comfort I could have would be the knowledge that I could access legal euthanasia when I decide the time has come. That I may be forced to take matters into my own hands while I still can fills me with fear.
Legal voluntary euthanasia is not ''Dr Death'' hovering over the bed of an unwilling victim. It is this type of fear-mongering from religious lobby groups that keeps nervous politicians from supporting it and gives those with religious views to which I do not subscribe control over my future. The last person I would want to see at the end of my bed would be a religious ideologue.
Name and address withheldAfter nearly 40 years of nursing, my advice to Nicholas Tonti-Filippini is that he moves on from his conservative and rigid views of healthcare provision. The nurse he would prefer to see at the end of his hospital bed may well be a ''him'' rather than a ''her''.
Graham Cadd, Surrey HillsIf only the lawmakers could understand the wisdom expressed so eloquently by Dr Peter Evans (13/5)
Jean Sands Sunbury
Article in The Age:
A doctor treating a patient who is terminally ill, or suffering intolerable pain, is faced with problems which few if any other professionals have to tackle.
There is now legislation which specifically permits euthanasia or assisted suicide in several American states, the Netherlands, Belgium, Luxembourg and Switzerland. The experience of these jurisdictions has provided very little, if any, evidence to support the objections of those who oppose a change in the law. But neither the Australian government, nor that of any Australian state, has shown any willingness to reform the law.
Murder occurs when a person by any deliberate and unlawful act causes the death of another person. The act would be murder even though the other consents, or was already dying or near death. It matters not that the other’s death was imminent. Nor does the act become lawful if the doctor believes he or she was acting in accordance with the wishes of the patient.
Suicide has not been an offence in Victoria since 1967. But Victoria’s Crimes Act provides that any person who incites another to commit suicide or aids and abets any other in the commission of suicide is guilty of an indictable offence, and liable to up to five years’ imprisonment.
Doctors’ problems start with their professional obligations, a reality in modern medical practice. Dying may be associated with intolerable suffering, the doctor has a duty to relieve suffering and respect patient autonomy, some suffering will only be relieved by death, and some patients rationally and persistently request assistance to die.
Sometimes palliative care cannot relieve all the pain and suffering of dying patients. The duty being to respect patient autonomy, the doctor may prescribe a dose of medication large enough to cause the death of the patient. Medical notes should then indicate the exact dosage given. But medical opinions may vary and others may take a different view of the likely imminence of the patient’s death, and form the opinion that the doctor’s primary concern must have been to hasten death rather than merely to palliate.
Or the doctor may have been observed by a suspicious nurse. A chance comment to a nurse or a family member may support the view that palliation was incidental to the main purpose. The doctor then runs the risk of a charge of murder, or aiding and abetting a suicide.
Where the doctor has actually administered the medication by injection, followed by the patient’s death, a charge of murder could be laid, as also if the drug was administered by another under the direction of the doctor. If the medication was prescribed or provided by a doctor and voluntarily taken by the patient acting with full mental capacity, aiding and abetting or inciting a suicide would be the appropriate charge.
On the other hand, if a patient demands the withdrawal or termination of treatment, a principal question becomes the mental capacity of the patient to make the decision.
The doctor’s dilemma, whether to take the risk of hastening death to relieve suffering, in conflict with the criminal law, may obviously arise in varying situations. For example, the prescription of deep continuous or terminal sedation, maintaining the patient in a continuing coma until death, may leave it open to be said that the sedation was the cause of the ultimate death. The possibility or probability of death can be foreseen in many occasions where this procedure is used, creating potential conflict with the criminal law.
Where doctors have been charged with hastening death, the usual instruction to the jury since Mr Justice Devlin tried Dr Bodkin Adams in 1957 has followed the line that the doctor is entitled to do all that is proper and necessary to relieve pain and suffering even if the measures taken may incidentally shorten life.
The absence of any relevant defence under the Crimes Act leaves the doctor exposed and at risk of prosecution in a variety of situations for at least aiding and abetting suicide.
If the community generally accepts that doctors not infrequently hasten the death of their patients to lessen their suffering, and at their request, juries may well be unlikely to convict an accused doctor who acted solely out of compassion, and at the request of a patient with full mental capacity.
In these circumstances the present state of the law is left in a quite hypocritical situation, in urgent need of change. An alternative defence for doctors in these circumstances many argue should be the defence of necessity. At the very least these issues demand to be referred to the Law Reform Commission for a full review and a clarification of the position of doctors.
As matters stand in Victoria, many doctors will, no doubt, continue to prescribe medication either for oral use or injection to those suffering intolerable pain near the end of life, notwithstanding that to do so may shorten their patients’ lives. But many others would understandably not be prepared to take the risks involved, leaving a number of their patients without adequate relief from their suffering.
And the aged and terminally ill in our community still have no right to make an informed decision as to the timing and manner of their death.
Stephen Charles QC is a former judge of the Court of Appeal and a member of Dying With Dignity.
Letters in The Age:
Much of the debate about end-of-life decisions refers to the ''victimisation'' of the elderly. This unfortunately continues the theme that older people cannot make clear, balanced, intelligent decisions about when and how their lives can come to an inevitable end. Older people aren't children who need to be protected from themselves by other, more-enlightened individuals. They are experienced, rational people who can make good decisions about their best interests. To act otherwise is to deny them their basic human rights. Of course support should be available to all people, but to force individuals to live a fully- or largely-supported life when they do not want that is unethical. We must acknowledge that death is inevitable. For those who wish to live on supported and those who don't, there is only one person qualified to take that decision - the person whose life is at stake. No one else.
Mary Edwards, KilsythThank you for your coverage about euthanasia. Dr Peter Evans explained beautifully the situation about dying being a lonely event (Letters, 13/5). My late husband spent his last few months in a constant struggle. He was a very proud man and to see him unable to talk, walk, eat, drink or look after his personal hygiene was heart-wrenching. Not only was this a struggle for him, therefore, but also for me as his wife. To prolong needless suffering is criminal. You tend to remember a person as you last saw them. I have enormous trouble trying to remember my husband as a healthy man, even though I have a huge collage of photos of better times hanging on the wall.
Paulien George, BerwickIrrespective of whether euthanasia becomes legal in Australia, quality palliative care should always be an option, but I fear the sector is already under-resourced. In March, my mother was admitted for two weeks of respite care into a well-respected hospice. This was where her in-home nursing care team was based. While there, her condition declined markedly. She had difficulty swallowing and required assistance to change position in bed. We had numerous conversations with doctors, pleading that she be allowed to stay. They refused, stating that as my mother entered on respite she must leave on the agreed date.
My dying mother was moved twice in the last five days of her life; from the hospice to an aged-care facility where staff were wonderful but not equipped to cater for her needs, and then to a geriatric medical ward in a private hospital. There, for 48 hours, she finally benefited from true palliative care. It is not as easy to come by as people might think. Bring on changes to laws governing end-of-life choices, but at the same time insist on adequate funding of palliative care services.
Lynda Moore, South MelbourneGraeme Duke is a good doctor: he cares and he does his very best for his patients (Comment, 14/5). Statistics support his statement that ''I admit I have been asked to hasten death. But in my experience this is surprisingly rare.'' In Oregon last year, where assisted dying is legal, only 0.2 per cent of those who died chose assistance. But 80 per cent in Australia want the choice. Dr Duke admits that ''too many suffer in their dying. One is too many.''
This is what the choice is about: the dying want the best medical and palliative care. But if that fails, 80 per cent want the last choice, their last right over their own dying bodies. They don't want to be the ''one too many''.
Janine Truter, The Basin
Article in The Age:
I will not accept dying at the end of a morphine drip in a drugged state. It would not benefit my family, my friends or me.
Illustration: Michael Leunig
My story is simple. I was diagnosed with oesophageal cancer five years ago and made a full recovery. Or so I thought.
On 28 January this year, my 57th birthday, I was told it had returned – terminally. At the time of writing, I have a prognosis of five months. I am hoping for a bit more than that, but it is clear I will die within months.
And I will die at the time I select. I respect those who believe it is better to hold on until the very end, whatever suffering that entails. Both paths are dignified. What is undignified is not having the choice.
I have become intimately aware of the debate raging around physician-assisted death and the right for people to choose the timing. Recently, Dr Rodney Syme, in The Age and elsewhere, has declared he has, in contravention to laws that should be changed, helped many terminally ill people end their lives.
Dr Syme is taking risks as he fights for decent and enlightened change. His advocacy has inspired me.
Dr Syme has, for the first time, admitted he gave a man called Steve Guest the drug Nembutal and the information on how to use it to end his life about 10 years ago. The case has eerie parallels for me. I have the same cancer Mr Guest suffered, and I even had a holiday house at Point Lonsdale, where he lived.
In the time I have left, I believe I must do what I can to fight for everybody’s right to freedom of choice to control life’s end process if facing a terminal illness.
This is not a legal, religious, moral, budgetary or bioethical issue for me, nor do I suggest it should be for you. It is simply about common sense, and compassion for people suffering physically, psychologically and existentially. I will not accept dying at the end of a morphine drip in a drugged state. It would not benefit my family, my friends or me.
I would like my last life scene to be one of great beauty and warmth – and perhaps even of inspiration for those around me and for me.
Many people fear death, often because of a lack of control. For decades we have put the dying, medical practitioners, law enforcement agencies and families of terminally ill people in an invidious legal and human situation. There has been so much unnecessary suffering. Choice is a powerful palliative force, I now know. There is an immediate and direct benefit from having end-of-life choice. It can restore some confidence and dignity to those whose circumstances have stripped them of autonomy.
Just knowing I have that choice vastly improves the quality of the life I have left. Dr Syme talks beautifully of this. Indeed, it is believed the majority of terminally ill people who are given the means and knowledge to end their lives actually do not use it.
And now I must face this labyrinthine, unfair system that blocks my right to choose. Some people fret that legalising physician-assisted death would create hazards. There are understandable concerns – for example, that people might be clinically depressed at the time they state they want the option of physician-assisted death or that some might be manipulated by greedy and unscrupulous relatives. But these issues can be dealt with effectively and carefully, as Dr Syme points out has happened in other places.
The reality for me is that after a lifetime of doing my best as a husband, father and member of the community, I now face a life-changing challenge to use the short time I have left to fight for change about which I am passionate. It should be of concern to us all – death is the only certainty.
The mandating of the right to choose end of life for the terminally ill is tragically overdue. I am doing this for my family and friends, for myself and for the entire community. It is also about passing on the experiences and insights I have had through living with cancer during the past five years.
Why have Australia’s lawmakers failed to have the decency and courage to reflect in statute what so many know: that compassionate medical professionals are, in effect, helping suffering people choose the timing of their death? The politics seems tortured and leaderless. Where are the politicians prepared to drive change? The current situation leaves the medical and legal systems in an excruciating, unconscionable limbo.
I have written a letter to seek a meeting with Prime Minister Tony Abbott. I call on him and Premier Denis Napthine, a vet by background who has surely euthanased a number of animals, to put in place a party position that the terminally ill should have access to physician-assisted death, with appropriate guidelines. I would like to meet with him to offer assistance.
Surely Victorians deserve at least the same respect and compassion as the animals Dr Napthine cared for. My wife and I said goodbye to a loved and dying cocker spaniel seven years ago in our home. The vet administered a lethal injection and my wife held and kissed Blue as she calmly drifted off.
It is wrong that I cannot choose to pass away with my wife's and sons' arms around me and a kiss on the head. As it stands, my prolonged death would probably be well-managed – I have a great medical team around me. But days or weeks in bed on debilitating doses of drugs, with me having no control, is not the way I will die.
I will go out of my wonderful life at a time of my choosing, with our dog Missi’s ear in my hand and my family by my side. I have met with Dr Syme, and he has given me the assurance I need around choice, and that helps underpin the calmness and joy I feel as I get to embrace the remainder of my thrilling existence.
To help others facing terminal illness, and to help ventilate and inform the struggle for the right to choose, I am writing a blog, and would welcome comments and questions: Peter Short's Blog

Letters in The Age:
I agree wholeheartedly with Peter Short on having the right to choose when to die (''Let there be no doubt, I will decide when I die'', Comment, 21/5), especially when one is in unendurable pain and terminally ill. I watched my beloved dog die quietly in my arms as I snuggled into her soft fur and thanked her for being in my life. The release from her pain was sad and beautiful as the vet injected her. We are all animals, some more intelligent than others, and we deserve to have that choice to die without prolonging agony or being in a comatose state. It's in our DNA to fight to live; I will not lose it unless I know there is no hope. I, too, would like to be in a favourite place with my loved ones at the end rather than hooked up to a drip. Let's use our intelligence to be kind to each other and legislate this right of choice to die. Other countries in Europe have done this, why not us?
Johanna Fairman, KallistaTo Peter Short (''Let there be no doubt, I will decide when I die'', Comment, 21/5): I want what you want.
Brian Sanaghan, West Preston
Article in the Sydney Morning Herald:
Victorian members of a pro-euthanasia group are fearful of police raids after warrants were executed across Australia over the importation of a lethal drug, group head Dr Philip Nitschke says.
Two people, from Western Australia and Queensland, have been charged with importing the illegal drug Nembutal, and state police have spoken to 10 others in WA, Queensland and South Australia in the past month.
Dr Nitschke, director of Exit International, said on Friday morning that the police action had spread a ripple of fear through the group's 6000 members, which include more than 1000 Victorians.
He said Victorians fear they are on a police hit-list and are concerned that police have accessed the group's database.
"Victorian members are saying they want to know if their information has been compromised," he said.
"It has caused a lot of alarm."
Dr Nitschke said the raids may also shut down one of the easiest ways people can access the drug, which is used by veterinarians to put animals down.
He said some of the group's members were able to order the drug online from a Chinese company and have it mailed to them.
"Members are very keen to access this drug, not because they're sick, but because they're getting on in years," Dr Nitschke said. "They think it's a very good idea to have this in place in case they might need it, in case they get to the stage where they're too sick and have to ask their husband or wife to do the ordering and the person assisting can be looking at very serious legal consequences."
Since the raids, Dr Nitschke said, the Chinese company had stopped supplying to Australia because it's "not worth it".
Rupert Ward, 69 of Albany, was charged about a month ago with possessing an illegal drug while Brisbane woman Lynn Afotey-Otu, 64, was charged with importation of the drug on Thursday last week.
Mr Ward will face a WA court next Thursday while Ms Afotey-Otu will face a court in Queensland on June 2.
For help or information visit beyondblue.org.au, call Suicide Helpline Victoria on 1300 651 251, or Lifeline on 131 114.
Article in the Herald Sun:
A POLICE investigation has begun into the deaths of two Melbourne women who obtained suicide devices from controversial euthanasia campaigner Dr Philip Nitschke.
A letter left by one of the women details their suicide pact. One of the pair had Alzheimer’s disease, but the other was healthy.
Detectives this week asked Dr Nitschke, known as “Dr Death”, to explain how the friends obtained equipment they used to die.
Viewbank housemates Val Seeger, 75, and Claire Parsons, 66, died in March, but their case was never made public by authorities.
In a note posted to Dr Nitschke and signed by both women, Ms Parsons said they decided to take their own lives after Ms Seeger was diagnosed in March last year.
Ms Parsons said that after agreeing to help her friend end her life, she felt existing laws left her no choice but to take her own life too.
Dr Nitschke admitted the women obtained equipment from him that he knew could be used as a suicide device. He said he had sold the equipment - which the Herald Sun has chosen not to detail - throughout Australia.
And Dr Nitschke has defiantly revealed plans to open a euthanasia clinic in Melbourne, having inspected a potential site in Essendon this week.
A coronial probe on the deaths “including whether this was assisted suicide” is also under way, Coroners Court spokeswoman Sheree Argento said.
Dr Nitschke said the women - friends for 24 years - took their lives.
It is understood Ms Parsons, an academic and published author, forwarded the letter, titled “I Have a Friend”, to Dr Nitschke, asking it be passed on to news media.
Dr Nitschke says he received the letter after the women had died.
Assisting a suicide carries a maximum five-year jail term in Victoria.
Six people have been prosecuted for their involvement in a suicide pact, inciting suicide and aiding or abetting suicide in Victoria since 1997.
Controversial euthanasia campaigner Dr Philip Nitschke. Source: News Corp AustraliaSenior Detective Emma Bennett, of Heidelberg CIU, said Dr Nitschke might be asked to make a statement in the investigation.
“The matter has to be thoroughly investigated to establish where they got (the equipment) from,” Sen-Det Bennett said.
Dr Nitschke said Ms Parsons felt she could not live without her best friend.
The two women were members of their local Exit International group.
Dr Nitschke, its founder and director, is a focus of three Medical Board of Australia inquiries.
“Suicide is not a crime. This is the only example of where assisting someone to do something lawful is a crime,” Dr Nitschke said.
“We are languishing in the dark ages here.”
Dr Nitschke, who has a clinic in Adelaide, said his proposed Melbourne advisory clinic would operate one day per month.
“It would be talking to people who are sick and considering what their options are,” he said.
His Voluntary Euthanasia Party was registered in Victoria yesterday. He hopes to run candidates at the election.
Anyone with personal problems can call Lifeline on 131 114.
WOMEN INTENT ON ENDING LIFECLAIRE Parsons could not be talked out of the pact she had with her best friend, euthanasia campaigner Philip Nitschke says.
Dr Nitschke said that people who had seen her the day before she ended her life reported that she was adamant, despite being perfectly healthy.
Her friend of 24 years, Val Seeger, was diagnosed with Alzheimer’s disease in March last year.
Dr Nitschke said the women were quite open about their plan at the last meeting of a local Exit International group they attended. He said Ms Parsons and Ms Seeger went to a euthanasia workshop in Melbourne in September, attended by about 300 people.
Ms Seeger was an award-winning and highly respected nurse.
Ms Parsons qualified with a doctorate in medical anthropology and did postdoctoral studies at Harvard University.
The pair volunteered with the Australian Red Cross emergency and disaster program for four years.
In a letter the women wanted distributed to the media, Ms Parsons wrote that after Ms Seeger’s diagnosis her friend said she did not want to be sent to a nursing home or lose her sense of dignity.
“She knows that she cannot wait too long and forfeit her ability to reason, as to ask for assistance would constitute homicide on my part, and neither of us believes that to be acceptable,” Ms Parsons wrote.
“Having said this, we are also aware that under the current (and we believe outdated) law in this land, the police are obliged to charge me with aiding and abetting a suicide and I am not prepared to undergo the harassment and disgrace of a prosecution.”
Ms Parsons wrote that their decision had been a rational one made by two people who had worked with people who have Alzheimer’s and who had a full knowledge of contemporary research in the field.
“We imagine that at the turn of the century, euthanasia/dying with dignity will be regarded as a normal, rational, ethical and legal action, accessible to all who wish to avail themselves of this option, while still protecting the vulnerable and their friends and family.”
EXTRACT FROM CLAIRE PARSONS' LETTER“Given the laws that exist at this time in history, what I am obliged to do, I will do, and do willingly.
“Who would consider a loyal friend to be someone who walks away when their friend is in need?
“What is loyalty when one abandons others in order to protect onself? I find I cannot do that.
“None of our actions has been taken lightly.
“But neither have they been taken with sorrow or regret.
“We are just two ordinary people, content and fulfilled with our lives but who have planned how to manage the disease confronting us and have chosen to leave this world before all dignity and integrity is lost.
“We will have a wonderful final day and share a meal together before we wish each other well on our final journey.”

Article in The Age:
Dr Philip Nitschke is being investigated by police after two women allegedly ended their lives with equipment supplied by the euthanasia campaigner.
Police are investigating the deaths of two Melbourne housemates who used suicide equipment provided by euthanasia advocate Philip Nitschke.
Viewbank housemates Val Seeger, 75, and Claire Parsons, 66, died in March in a suicide pact.
Ms Parsons, who was healthy, had agreed to help carry out her friend's wish to die after she began showing early signs of dementia, Dr Nitschke said.

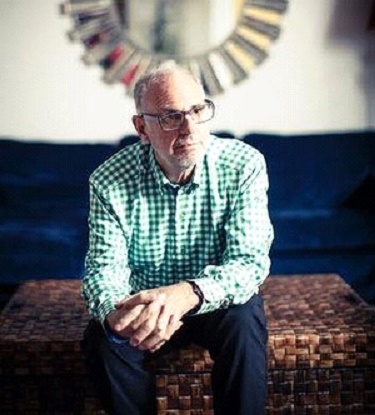
Dr Philip Nitschke, the director of pro-euthanasia group Exit International, said the deaths were in a "murky" area between suicide and euthanasia. Photo: Kate Geraghty
Laws prohibiting assisting a suicide, and the thought of living on without her best friend, had spurred Ms Parson's decision to also die, he said.
"Claire said she couldn't live with the risk of criminal charges for assisting suicide ... and she said Val is my closest friend and I don't really want to go on without her," Dr Nitschke said.
The pair, who had been friends for more than two decades, had sent a letter to Dr Nitschke saying they had decided to take their own lives, and asked that it be circulated.
Heidelberg police this week questioned Dr Nitschke over the deaths.
Dr Nitschke said he has admitted providing the equipment, which is legal, but can be used for suicide. "I've answered all their questions," he said.
Fairfax Media has obtained a copy of a letter written by Ms Parsons before her death.
In the letter, Ms Parsons says her friend was suffering from the onset of Alzheimer’s disease and due to her background as a health professional sought to avoid an ‘‘undignified end’’.
She also outlined why she decided to join Ms Seeger in taking her own life.
‘‘Under the current (and we believe outdated) law in this land, the police are obliged to charge me with aiding and abetting a suicide and I am not prepared to undergo the harassment and disgrace of a prosecution,’’ the letter reads.
‘‘This leaves me no choice but to join my friend at her time of death.’’
The maximum penalty for assisting suicide in Victoria is five years' jail, but in other jurisdictions it is life imprisonment.
Dr Nitschke, the director of pro-euthanasia group Exit International, said the deaths were in a "murky" area between suicide and euthanasia.
He said prosecutors in the UK were able to consider compassionate circumstances in cases of assisted suicide.
"I think there needs to be a look at ways of dealing with these compassionate acts ... when someone feels obliged to help someone they love or care a great deal about then they shouldn't find themselves subjected to these penalties."
Dr Nitschke said the two women were prominent Victorians – Ms Parsons was a renowned medical anthropology academic and published author, and Ms Seeger a highly respected nurse.
The two women were members of their local Exit International group.
Dr Nitschke said the women had spoken about their suicide pact at their last Exit International meeting.
A Victoria Police spokesman said police investigate all unsuspected deaths for the Coroner.
"If a death is deemed non-suspicious, then a brief is prepared for the Coroner," he said.
"The Coroner may direct police to investigate further or may make a finding based on the available evidence."
For help or information call Suicide Helpline Victoria on 1300 651 251 or Lifeline on 131 114, or visit beyondblue.org.au

Article in The Age and Sydney Morning Herald:
 />
/>Peter Short, advocate for physician-assisted death, talks with the Zone's Michael Short.
[WHO] Peter Short, terminally ill cancer patient campaigning for physician-assisted death.
[WHAT] Dying people have the right to choose how and when their life ends.
[HOW] Mobilise community support to prompt a change in the law.
This is about you. While it is the story of a terminally ill man who has been told he will die within months, it is equally about you and your death. Today's guest in The Zone is not here because he is dying, but because of how he is living.
Husband and father Peter Short is spending a significant slice of his remaining time on this earth campaigning for legalisation of what he and so many others believe is the right of terminally ill people to choose when and how they die.

''It is wrong to be in a position where at the end of your life you are prevented by the laws of the country that you've lived in your whole life to have an exit process that you can control.
''You read the statistics around people's desire to have choice at end of life, and it seems to be that 70 per cent to 80 per cent of Australians would like to have that choice made available. You have a political system that won't talk about it, and you have the fear of death that nearly everybody has.''
On his 57th birthday in January, Peter was told the oesophageal cancer with which he had been diagnosed five years previously, and of which he thought had been cured, had returned and was terminal. He was told he would die within about nine months, and perhaps had as few as three months left.
A video statement by Peter and the full transcript of our discussion can be found at theage.com.au/federal-politics/the-zone. He will be online for an hour from midday to respond to questions and comments, which can be submitted from this morning.
Although he had believed in medically assisted death all his adult life, Peter's decision to campaign for it did not come until several weeks after his diagnosis.
Medically assisted death, also known as physician-assisted death, refers to a doctor giving a dying patient the medical means and knowledge to end their life peacefully and painlessly.
Peter was moved to act by reading in The Age about Dr Rodney Syme, who has been campaigning for the right to choose medically assisted death and who has been defying the law for years by helping terminally ill people die.
In the article, Syme, who had discussed the issue in detail in The Zone in 2011 (see link below), stated he had about 10 years ago helped a man called Steve Guest die by giving him access to Nembutal, the drug veterinarians use to euthanise suffering animals.
By making these public admissions, Dr Syme is challenging the authorities to arrest him. Although he has some apprehensions about submitting to the stresses of the court system, Syme is prepared to risk conviction, such is his belief that the law needs changing - as it has been in a number of nations.
The story particularly resonated with Peter because he has the same cancer that Steve Guest had. Guest also lived in the Victorian coastal town of Point Lonsdale, where Peter had a holiday house.
''When I read that article, it just called out to me. The ability to have choice at end of life was something that I felt compelled to get involved with.
''When you're actually sitting there having a [palliative care] plan that says eventually I am going to be managed out with morphine, which will be the end of my life, it just seems wrong.''
Spurred by what he considered Syme's courage, Peter wrote an opinion piece (see link below) in The Age, in which he stated: ''Dr Syme is taking risks as he fights for decent and enlightened change. His advocacy has inspired me …
''In the time I have left, I believe I must do what I can to fight for everybody's right to freedom of choice to control life's end process if facing a terminal illness. This is not a legal, religious, moral, budgetary or bioethical issue for me, nor do I suggest it should be for you. It is simply about common sense, and compassion for people suffering physically, psychologically and existentially.''
In that piece of writing and in our discussion for The Zone, Peter stresses that both the option of medically assisted death and of letting death come when it might are dignified. What he considers undignified is not having the choice.
''Dignity means being able to represent yourself and conduct yourself to those around you in a way you believe you should be seen and should be dealt with. I've thought deeply about this since Rodney Syme sparked me.''
Opponents to medically assisted death argue there is an unacceptable risk that terminally ill people might be depressed at the moment they are seeking choice, and thus could end up doing something inappropriate. They also argue that greedy, unscrupulous relatives might manipulate ill relatives into an early death.
Syme and other advocates say international experience shows these concerns can be readily dealt with in legislation and in practice.
Peter has set up a blog, Tic Toc Tic Toc dying to a killer clock , to document his experience, ventilate his campaign and facilitate community discussion.
''I received a very long email that had me in tears from a Dutch lady who has been involved with her father's death in Holland. She explained to me the process that he went through - the doctor coming to certify that he was OK and he was of the right mind to do this, and how he died. It was a peaceful, beautiful death. That is a case of a country that is managing some of these outlying things with sensible laws.''
Syme and other advocates for medically assisted death argue one of the strongest reasons to change the law is that simply giving terminally ill patients the means to end their life immediately improves their quality of life.
Peter's experience is testament to this notion. ''[Having] the choice becomes incredibly powerful. The important thing to me is that I have come to realise that having that choice takes a burden off me, which is extremely palliative in its own right.''
Like so many others who have been given the choice by doctors who, like Syme, feel morally compelled to break a law they believe causes massive undue suffering, Peter is not sure he will ultimately take the option. Doctors say a majority of people who have the option of medically assisted death do not select it.
What is important to Peter is that if and when he asks, Rodney Syme will give him the assistance he needs to end his life. He is buttressed by his confidence in, and regard for, Syme.
''He is such a generous-spirited, humane, warm, well-intentioned and super-intelligent man who has been working to try to help people through giving them choice for years and years of his life. I have got a huge respect for him.
''If I choose to have him help me, and therefore avail myself of choice … I trust him implicitly that when I choose that, he will support it.''
Peter is determined not to ebb away - semi-conscious until increasingly large doses of morphine end his time.
''I want the end to be something as special as it can be, although it is a dire and sad circumstance for all of those around me. But I also have an excitement around dying, not that I am rushing towards it. I have a belief that the body and the mind is an amazing thing.
''I can't believe that as one is going through the final movements of their life, there is not going to be chemicals running around inside your body giving you an opportunity to probably have a quite exceptional experience.
''It may be an insight, it may be your brain just opens up to a depth you never knew was possible and in milliseconds you can see hundreds of thousands of things you never believed possible. So, I am looking forward to how do I make those last moments as magical as possible, and what is my body going to be capable of doing in them.''
Peter has written to Prime Minister Tony Abbott and Victorian Premier Denis Napthine seeking a meeting. He has heard nothing back from these lawmakers. ''I am disappointed at a very deep level that they have not got the respect to actually pick up a phone and talk to me.''
He does not believe, anyway, that politicians will lead change on this issue. ''I think they're uncomfortable opening the topic up because looking anyone in the eye and talking about dying and how people should die et cetera is a very confronting and emotional topic.''
He believes, too, that politicians have acute electoral antennae, so he is focusing his efforts on mobilising community support for a change to the law. As part of that, he has launched an online petition, which can be accessed through his blog.
Peter knows he will not live long enough to see the change he is seeking. So, he is imploring people to act.
''I am looking for the community to think through a really, really important issue and make a call and do the unusual, which is then actually stand up and make a whole lot of noise about it rather than thinking, 'It's a very, very busy world and, yes, I understand the campaign and hope it does well'.
''What I really want is for them to actually make a difference.''
Michael Short is Peter Short's cousin.

Letter in The Age:
The decision to die taken last week in WA by an elderly couple with intolerable suffering is a further reminder that our legislation is lacking. This couple could not consult anyone, including their doctor, about choosing to die because the other party might be seen as criminally liable for assisting suicide. Even to discuss methods of suicide on the telephone, via letter or email is a federal crime. Well-considered legislation would protect the families and doctors of those at the end of life, allow questions to be asked and answers to be given without fear of prosecution, and, perhaps, longer lives to be lived with the knowledge that a death with dignity was a right, not a crime.
Janine Truter, The Basin
Article in WAtoday:

Dr Philip Nitschke's support of a Perth man who committed suicide has drawn the ire of Jeff Kennett.
The suicide of a young, healthy West Australian man supported by euthanasia campaigner Dr Philip Nitschke has escalated debate around assisted life-ending and triggered concern a dangerous line has been crossed.
As news broke that in May 45-year-old Perth man Nigel Brayley took the illegal drug Nembutal and contacted Dr Nitschke before taking his life, the response from one of Australia’s leading mental health support groups, beyondblue, was swift.
Beyondblue chairman and support group founder Jeff Kennett labelled Dr Nitschke’s involvement in Mr Brayley’s death as “offensive” and a “gross breach” of the medical profession's ethical standards.
“This man did not have a terminal illness and Dr Nitschke’s actions are a gross breach of his Hippocratic Oath as a doctor, and offensive to all standards of common decency," Mr Kennett said.
“Equally unacceptable is Dr Nitschke’s comment that he did not see it as part of his responsibility to refer the young man to an appropriate specialist for further treatment.
“So our GP detects we have cancer and does not refer us to an oncologist? Our GP detects we have a mental illness and does not refer us to a psychologist of psychiatrist? Dr Nitschke says ‘no, support a young individual to end their life’.
“In my 14 years leading beyondblue, I know our team, our work, together with many other such organisations, have saved and repaired many lives. We exist to improve the quality of life for Australians, not end it."
Mr Kennett said Dr Nitschke's involvement with Mr Brayley had done "a great deal of harm" to his more general cause for euthanasia.
“Millions of dollars are being spent by governments and community organisations, correctly to reduce suicides in Australia," Mr Kennett said.
“The latest preliminary figures released by the Australian Bureau of Statistics for 2012 indicate 2535 Australians took their own lives that year, which equates to seven deaths a day – twice our road toll.
“That figure is unacceptable, and we are all working to reduce it, except it seems Dr Nitschke who seems to be working to add to those numbers.
“Dr Nitschke has coined the phrase ’rational suicide’ to justify his involvement in this case, and we hear he wants to have a conference next year in Australia on the subject.
“I do not mind discussion, and I am happy to participate in debates putting a contrary point of view. But that is very different from direct action that assists the ending of a life of an able bodied person.
“As a long-time supporter of euthanasia for the terminally ill, for those for whom the dignity of life has been lost, and under special conditions, I believe Dr Nitschke’s latest act has crossed the line of decency and professional conduct.
“I trust the appropriate media board or boards and governments will move quickly to investigate Dr Nitschke’s latest act.
“He has done society a great disservice and in my opinion should no longer be registered to practise as a medical professional."
Mr Brayley came to public attention when his wife Lina was found dead at the Statham’s Quarry, Gooseberry Hill, in February 2011.
The body of Ms Brayley, an amateur photographer, was found at the base of the quarry with her camera equipment nearby and initially ruled an accident.
Two years later WA Police believed her death was a homicide and launched a public appeal for information.

Letter in The Age:
The unresolved question at the base of the controversy surrounding the death of Nigel Brayley (''Nitschke's actions offensive: Kennett'', 5/6) is can rational people have suicidal thoughts and in some cases act on them? Traditionally, suicide has been stigmatised by implying that all those who consider it are in some way mentally unbalanced and in need of medical help. But do all those who attend an Exit International meeting need psychological or psychiatric assistance? Most are respectable and sensible people merely interested in exploring options. In fact, it might be the calm, measured and rational approach that increasing numbers of Australians now take to their own deaths which so upsets people such as beyondblue's Jeff Kennett and AMA president Brian Owler.
Rod Wise, Glen Iris
Letters in The Age:
It was good to read that beyondblue chairman Jeff Kennett - while blasting Dr Philip Nitschke's act of aiding an unhappy but apparently healthy man's suicide - supports voluntary assisted dying for the terminally ill (Saturday Age, 5/7).
The Dying With Dignity movement is about establishing strict rules and guidelines under which assisted dying can be legally practised - but only for terminally or incurably ill people who request it, and only by doctors who believe it is justified. Greens senator Richard Di Natale has tabled a draft bill for a Medical Services (Dying with Dignity) Act. Its provisions would not enable Dr Nitschke's recent act, nor set society onto a slippery slope into abuse. It would just relieve much anguish among a significant number of ill people who dread what they may have to endure before their deaths.
Anne Riddell, Mount MarthaIn helping 45-year-old Nigel Brayley - who was suffering from depression but who did not have a terminal illness - to die, Philip Nitschke has disparaged the Hippocratic oath and deserves to be deregistered as a doctor.
David Seal, Balwyn NorthAustralian Medical Association president Brian Owler says: ''A patient who has suicidal ideation deserves the opportunity to seek help, to be treated and supported. It has nothing to do with a debate about euthanasia … to suggest a doctor might vacate their obligation to provide support and care for a patient.''
Many would disagree that the current controversy has nothing to do with euthanasia. Dr Nitschke, and many other medical and lay people around the world, has sought to encourage a more rational attitude to ''dying with dignity'' and for people to have more rights in managing their own departure from life.
In Holland, these rights have been written into law. Horrifically, when our own Northern Territory voted for and established such law, Federal Parliament overthrew it. It is amazing that we continue to castigate as ''offensive'' the efforts of someone who is concerned with the welfare of people and assists those who want to leave this life.
Neville Rutledge, KewI am opposed to euthanasia, but have not been able to say so out of sympathy for the cases of terminal illness.
Now, the ''slippery slope'' has arrived. If euthanasia is legalised, confining it to the old and terminally ill is arbitrary.
It is not only the helplessness and pain of illness that can rob a person of their dignity. A prognosis of ''terminal'' is not the only form of hopelessness. There are many reasons why someone believes no life is better than the life they have, and the one they have to look forward to. They may wish for a more dignified way out than suicide. We now see how hard it is to draw a line.
Gavan O'Farrell, OakleighPhilip Nitschke's comparison of ''ticking a box'' at the airport with ticking the box on the Exit International website is ridiculous. An airport does not just assume you are telling the truth. There are checks and balances, such as scans, detectors, passports, photo ID. Can Exit International say the same?
Kathleen McGee, Mount Eliza
Editorial in The Age:
Life is inestimably precious and should be protected - but not at all costs. Many terminally ill people suffer dreadfully, physically and psychologically, as their death draws near. This newspaper believes such people have a right to physician-assisted death, also referred to as voluntary euthanasia, in strictly defined circumstances, including that they are certified to be mentally well when they make their decision. Polls show that as many as four in five Australians support assisted death.
But The Age does not support euthanasia advocate Dr Philip Nitschke, because, through his organisation, Exit International, he aids people who are not terminally ill to die by suicide. We applaud the Medical Board of Australia for suspending Dr Nitschke from practising medicine over his alleged handling of a troubled man who sought advice about how to end his own life. Nigel Brayley, a physically well 44-year-old Perth man who was under investigation for his alleged involvement in the 2011 death of his wife and the 2005 disappearance of his former girlfriend, died in May after taking a fatal overdose of a drug discussed at Exit International forums. Other supporters of assisted death, as well as mental health experts, have also backed the censure of Dr Nitschke.
It would be a shame were opponents of assisted death to seize on DrNitschke's behaviour as an argument against reforming laws that, inVictoria, make it a criminal offence, carrying a maximum penalty of five years' jail, to aid or abet death by suicide. As we have repeatedly argued, the issue of physician-assisted death ought to be referred to the Victorian Law Reform Commission, which should formulate prudent proposals that can be then adopted by Parliament. While politicians must be the ones to pass legislation, putting the substance of the matter in the hands of the commission would help to depoliticise the debate and pave the way for change the community clearly and rightly wants.
At the federal level, draft legislation that would permit strictly controlled voluntary euthanasia has been tabled by Greens senator Richard Di Natale. He has been moved in part to act by the entreaties of a 57-year-old terminally ill Victorian man, Peter Short, who has been campaigning for his right to die at a time of his choosing since being diagnosed in January with oesophageal cancer and told he had between three and nine months to live. We urge all federal parliamentarians to carefully consider Senator Di Natale's bill.
Mr Short is dying from the same illness that caused another Victorian man, Steve Guest, to end his own life almost a decade ago with the assistance of Melbourne urological surgeon, Dr Rodney Syme. Dr Syme, who has not been arrested, has recently openly tested the law by stating he helped Mr Guest and a number of other terminally ill people to die. Dr Syme is not seeking the stress of being tried in court, but rather is compelled by compassion. His logic is unimpeachable: there can be a crescendo of suffering as death draws nigh; a doctor's duty is to relieve suffering; some suffering will only be relieved by death; a doctor's duty is to respect a patient's autonomy; some patients rationally and persistently request assistance to die; palliative care cannot relieve all the pain and suffering of dying patients. Simply giving patients the choice can improve their wellbeing - and Dr Syme's experience shows that many end up not taking the option.
Other nations have passed legislation that allows medicos like Dr Syme to offer peace to terminally ill patients but prevents those like Dr Nitschke from facilitating the death of people who should instead receive treatment.
Australian lawmakers should respect the right of terminally ill people to make informed choices.

Letter in The Age:
Dr Simon Smith (Letters, 25/7) is right in suggesting the Medical Board of Australia has taken an inconsistent position in suspending Dr Philip Nitschke but not Dr Bruce Reid. Perhaps more importantly, the board's decision implicitly encourages the view that euthanasia is wrong in principle. The decision encourages the human tendency to simply divide difficult issues into binary opposites, such as either right or wrong. Euthanasia, however, cannot be so divided; it is a complex issue. More and more people in our community have begun to recognise the complexities involved and want a meaningful debate. It is no longer good enough to have one body with vested interests dictating so-called ''rights and wrongs'' of an issue that may well involve each one of us directly or indirectly. Meaningful debate, that is willing and able to deal with the very real complexities of euthanasia, is urgently needed.
Lesley Cowie, Blackburn

LINKS



Red Jos: HUMAN RIGHTS ACTIVISM
Mannie and Kendall Present: LESBIAN AND GAY SOLIDARITY ACTIVISMS
Mannie's weblogs may be accessed directly by clicking on to the following links
Activist Kicks Backs - Blognow archive re-housed - 2005-2009
RED JOS BLOGSPOT (From January 2009 onwards)

This page created on 11 JUNE 2014 and updated 7 JULY 2021
PAGE 83