




Article in The Age:

Victorians may be able to access voluntary euthanasia in the near future, after Health Minister Jill Hennessy declared she supports it and that the parliament and Labor government had to look at the issue closely.
Earlier this year a cross-party parliamentary inquiry recommended Victoria introduce voluntary euthanasia.
Euthanasia around the worldAdvocate Andrew Denton on Australia's crucial role in spreading euthanasia laws around the globe.
As Health Minister, Ms Hennessy is responsible for the Andrews government's response to the inquiry, which is due by December 2016
"I believe that as a government, and as a parliament we need to look at euthanasia very closely," Ms Hennessy told Fairfax Media.

"Personally – and I believe personal experience plays a strong role in informing people's views on this issue – I support euthanasia."
"I also think it is clear community sentiment has shifted on this issue, and there is significant community debate around euthanasia at the moment.
She said as responsible minister she was carefully examining all of the committee's work and that if Labor did pursue euthanasia proper safeguards would be put in place.
On Tuesday the Andrews government introduced new laws to parliament to make advanced care directives legally enforceable.

In the strongest indication yet that Labor may introduce laws to allow euthanasia, Ms Hennessy did not rule out a scheme when pressed on Tuesday, saying the inquiry had widely canvassed community views and that of the medical and a legal professions.
"I don't have a religious or ethical objection to euthanasia," Ms Hennessy said.
"There are great opportunities for us to provide a better death for Victorians."
She said the inquiry's recommendation around an assisted death scheme was something she had "a very open mind" towards, but the decision was ultimately for the whole government.
"I think the material canvassed in the inquiry is very good."
Labor introduced new laws on Tuesday to parliament to make advanced care plans legally binding.
The directives currently give patients the power to set certain terms and guidelines for their doctor at the end of life but are not enforceable.
The new laws will make it clear for health professionals what a patient's preferences are, and for the first time in Victoria make breaching these preferences a matter of misconduct, with deregistration a possibility.
The bill states that patients cannot reject palliative care because of clinical feedback that not all people understand what pain and death is actually like, Ms Hennessy said.
The law will apply, with rigorous checks and balances, to children as well.
"We've put some carrots and sticks in the bill," she said.
The conversation people have around their death needs to become more culturally acceptable, with Ms Hennessy calling on more Victorians to talk with their GPs about death.
"We want to change the culture around people not having these conversations around a barbecue or a dinner party table. We want them to happen with their GPs and clinicians and to commit an advanced care plan to writing," Ms Hennessy said.
There will also be safeguards around a person's level of mental capacity in making an advanced care directive, with power of attorney laws.
The minister said there was not enough policy focus on the end of life.
"Our historic new laws will give Victorians the certainty they want and need when it comes to end-of-life care and wishes," Ms Hennessy said. "We're putting people's preferences and values first when it comes to medical treatment decision making."
Dying with Dignity Victoria welcomed the fulfilment of Labor's election commitment.
"This and changes to palliative care services to meet community expectations represent a significant step forward," said Lesley Vick, DWDV president.
"The framework recognises that current practices do not meet community expectations, notably that many people wish to die at home but are unable to do so," she said.
Any euthanasia laws would be subject to a conscience vote on both sides of politics.
Greens MP Colleen Hartland said the government needed to introduce euthanasia laws as soon as possible and if the government failed to do so, the party would introduce a private member's bill.
"There is overwhelming support for assisted dying to be made legal. The government needs to step up to the mark and give terminally sick people the power to end their suffering," Ms Hartland said.
"We welcome people being given control over medical decisions through advance care plans, but want terminally sick people to also be given the choice to end their lives."

A Melbourne doctor who has given scores of sick people a lethal drug has won a fight against the medical board, with a tribunal ruling his practise is consistent with other forms of palliative care.
In an extraordinary decision that could set a precedent for other doctors wanting to help patients die, the Victorian Civil and Administrative Tribunal has ruled Dr Rodney Syme does not pose a risk to the public, even though he has given about 170 people a drug that they used to end their own lives.

Dr Rodney Syme (left) and Bernard Erica, who is dying of cancer. Photo: Penny Stephens
In January, the Medical Board of Australia took urgent action against Dr Syme after it was told he was planning to give Nembutal to Bernard Erica, a 71-year-old Brighton man who was dying of tongue and lung cancer. Mr Erica had sought Dr Syme's help because he wanted to die at home and have control over his own death.
Upon learning of this, the board ordered Dr Syme not to "engage in the provision of any form of medical care, or any professional conduct in his capacity as a medical practitioner that has the primary purpose of ending a person's life".
The order was made on the basis that Dr Syme, an 81-year-old urologist and vice-president of Dying with Dignity, posed a serious risk to people, including Mr Erica.
But Dr Syme challenged this in VCAT last month, arguing that his provision of Nembutal to people with intolerable suffering was not done with the primary intention of ending their life, but rather to relieve suffering and to give people control over their death.
His lawyers argued that this was consistent with the doctrine of "double effect" in medicine which permits doctors to administer drugs or other treatments to relieve symptoms even if there is a secondary consequence of hastening death.
Dr Syme told the tribunal he had counselled about 1700 people with terminal illnesses or intolerable suffering over many years, and had provided about 10 per cent of them with Nembutal. He estimated about 40 per cent of them actually took the drug to end their life, and that all of them benefited from knowing they had the option.
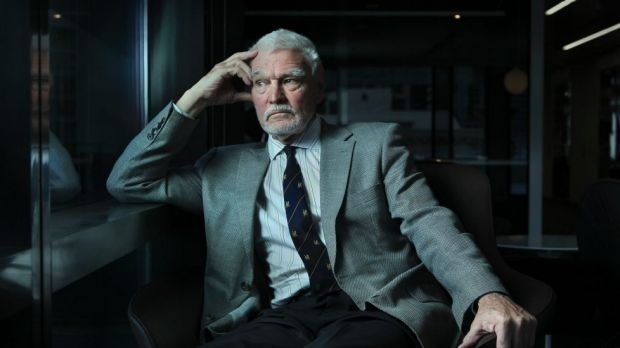
Dr Rodney Syme is vice-president of Dying with Dignity. Photo: Simon Schluter
Two palliative care specialists backed Dr Syme in the hearing, indicating that it was only their understanding of current law that kept them from doing what Dr Syme does. One said that it if was legal to prescribe Nembutal, a drug used to put animals down, he would do so for some people.
After hearing evidence from Dr Syme, Mr Erica, and the two palliative care experts, the tribunal ruled that Dr Syme's intentions were consistent with the Australian Medical Association's advice to doctors that all patients have a right to receive relief from pain and suffering even where that may shorten their life.
It also said that Dr Syme's provision of Nembutal to patients he deems to be rational was analogous to the process of terminal sedation where a mixture of opioids and sedatives are used at the end of life. This is sometimes done by palliative care doctors and is not considered to be physician assisted death or euthanasia.
The tribunal said it accepted Dr Syme's "frank and comprehensive evidence" and said he demonstrated extensive and relevant experience and expertise in counselling terminally ill patients; was relevantly informed about palliative care; and knew when to refer people to psychiatric care.
The tribunal accepted Dr Syme's evidence that when promising or actually providing Nembutal, his intention was not for the primary purpose of ending that person's life, and that if they do ingest it, it is a secondary consequence consistent with the double effect.
"In the tribunal's view, consistent with the opinions of both experts, the choice of a rational patient who elects to end their life rather than endure intolerable suffering and an uncertain death by means of other palliative care options, is not a death which can be described as harmful for the patient," it said.
"In the tribunal's view, on the evidence there is no basis to form a reasonable belief that Dr Syme poses a serious risk to persons."
It overturned the order on Dr Syme's medical registration. Dr Syme welcomed the finding and said it "completely vindicated" his work. He urged Victorian MPs to read the judgment ahead of a conscience vote on an assisted death law for Victoria due to take place next year.
If you are troubled by this report, you can call Lifeline on 131 114 or beyondblue on 1300 224 636.
The Victorian Upper House Committee of Inquiry into End of Life Choices produced an excellent report last year, which stated that "the current legal framework is not serving Victoria well", and recommended that the government legislate for assisted dying with appropriate safeguards (which it broadly described). In response, the government announced it would introduce legislation in 2017, and wisely determined to move cautiously, appointing an expert ministerial advisory panel, chaired by a former president of the Australian Medical Association, Brian Owler.
The only disappointing aspect of the parliamentary report was the recommendation assistance in dying only be available to people who were within "weeks or months" of dying. The other determinant was that the person was suffering from "a serious and incurable condition which is causing enduring and unbearable suffering that cannot be relieved in a manner the patient deems tolerable".

A fundamental difficulty for the panel is that these two conditions are in conflict in two fundamental ways. The first is that "serious and incurable conditions" are not confined to those with only weeks or months to live – essentially people who are terminally ill, or to be more specific, actually dying (in the terminal phase of a terminal illness). The second is that "enduring and unbearable suffering" is not confined to those with "weeks or months" to live. The evidence of the Victorian coroner, upon which the inquiry placed great weight, reveals that at least half of the three to four Victorians a week who because of a serious medical condition commit violent suicide do not have only weeks or months to live. They had what I describe as an "advanced incurable illness" – note the similarity to "a serious and incurable illness" cited by the inquiry.
They are people with chronic organ failure in the broadest sense. It is not difficult to comprehend that people with chronic heart or respiratory failure, perhaps reliant on continuous oxygen, suffering from fatigue, diminished mobility, pain, and, most importantly, severe breathlessness, have a serious and incurable illness, but their trajectory to death is unpredictable. Similarly, people with neurological failure, such as multiple sclerosis, motor neurone disease and Parkinson's disease, who have progressive diseases, and those with profound stroke or high quadriplegia who have a static condition, may have an ill-defined trajectory to death, and while suffering unbearably, may be discriminated against by narrow legislation. There are other uncommon examples of chronic organ failure of the urinary and gastro-intestinal systems (particularly in relation to continence) and musculo-skeletal systems (predominantly chronic poly-arthritis) which also deserve consideration.
The critical point is this: confining assistance to those with "weeks or months to live" is discriminatory, and will leave many people to suffer intolerably, and perhaps continue to take their own lives in a violent manner. And it will not resolve this issue from a medical perspective; these people will still attempt to engage with their doctors for assistance, and those doctors with empathy and compassion will still find it either impossible to help ease their deaths, or will continue to act outside a law that is not effective.
The essential problem is that terminal illness is a vague and difficult to define concept, and intolerable suffering can occur outside this frame. Finding a form of words that is neither too narrow and discriminatory nor too broad is the difficult task for the panel and the government. Mental illness and those without competence (for example, dementia) are already excluded.
It is important for legislators to understand that this is a matter that goes beyond physical pain to other forms of physical suffering, and, equally importantly, to associated psychological and existential suffering. Many politicians in 2008, when this issue was last debated in the Victorian Parliament were perplexed by the term "existential" in relation to suffering. It relates to our existence as human beings and to those fundamental things that give us quality of life – independence, pleasure, purpose, and a sense of control over our life.
The panel and the government should take note of the two most important safeguards against abuse – both incapable of being defined in legislation, but of fundamental importance in argument and practice. First, people do not want to die; they will fight and hang on to life as long as they can. A request for assistance to die only comes from, and is acted upon, in situations of extreme suffering – give suffering people the control and they will not use it unless there is no alternative. Second, the medical profession is the guardian of people's lives, and will not act to assist without extreme caution, and in clearly defined circumstances.
Dr Rodney Syme's new book is "Time to Die" (MUP). In recent days he was recognised as Australian Humanist of the Year for 2017 by the Council of Australian Humanist Societies.

From Daily Maverick

In life, one of South Africa’s most prolific and celebrated historians, novelists and translators, Karel Schoeman, was notoriously hermitic, shunning most contact with the outside world. Schoeman, who worked as an archivist at the National Research Library before he retired, led a rich inner life, populated by little-known voices and characters of South African history whom he honoured in his delicate, accomplished writings. But Schoeman’s self delivery – or suicide – on Monday at the age of 77 has once again opened the debate about the legal right to die with dignity in South Africa. He wanted it that way.
Accepting the Alan Paton Award for non-fiction in 2014, journalist, commentator and author Max du Preez remarked that it was really Karel Schoeman who should have been the recipient of the award. Schoeman, said Du Preez, was one of his “all time heroes” who had influenced Du Preez’s thinking.
“I only came tonight because I thought I was going to meet Karel Schoeman. And then he didn’t come! Which has kind of destroyed my night. But Karel Schoeman is one of my all-time heroes. He’s influenced my thinking, I envy his knowledge and his commitment. This really should have gone to him. He’s a spectacular guy. I’m sorry to miss him once again. He doesn’t return my phone calls or my e-mails. For 25 years.”
That was Schoeman.
Prolific and versatile, Karel Schoeman wrote 19 collections of prose and some 46 works of non-fiction, biography, historical writing, autobiography and travel, covering 300 years of South African history and establishing a unique and engaging style of interpreting this past. He wrote, like some of his characters, for those who could not.
Schoeman's literary landscape was vast and wide. He wrote about the history of Bloemfontein, Scotland, biographies of Olive Schreiner, Irma Stern as well as penning historical masterpieces including titles such as The Griqua Captaincy of Philippolis, Early Slavery at the Cape of Good Hope and Seven Khoi Lives: Cape Biographies of the Seventeenth Century.
His works of fiction, while often engaging with the past and history, were also about the inner journey of the protagonists within a specific geographical and historical landscape.
Years ago, when he still worked as an archivist at the National Research Library in Cape Town, Schoeman, with his full head of grey hair and goatee beard, could often be spotted purposefully striding to work through the Company’s Garden. His “office” was in the basement of the library, a wondrous treasure trove of documents and material that would form the essence of so many of his books, all of which were meticulously researched.
Schoeman was a maverick, a man outside of his time. After matriculating from Paarl Boy’s High in 1956 he obtained a BA degree in languages from the University of the Free State. Then, in 1961, Schoeman joined the Franciscan Order in Ireland as novice for the priesthood, but returned to Bloemfontein to obtain a Higher Diploma in Library Studies in 1983. Prior to this he had worked as a nurse in Glasgow and a librarian in Amsterdam.
Perhaps the younger Schoeman, in seeking the priesthood, had hoped to inhabit the hermitic and ascetic life he would later fashion for himself back in South Africa.
Schoeman at once belonged in the world but was not of it. If he could have asked a genie for one superpower it probably would have been the ability to render himself physically invisible apart from the manifestation of his writings.
And on Monday, May 1, Schoeman did just that shortly after delivering, by e-mail, the closing chapter of his final manuscript to his publishers with “Final Greetings (Laaste Groete)” in the subject field. The book is expected to be published in September.
Schoeman, who was born in Trompsburg in the Free State in 1939, died in the Noorderbloem retirement home in Bloemfontein. He was 77 years old. In a letter to his lawyer, composed on 27 April and simply titled “Statement”, Schoeman set out how he had long planned to end his life before he grew too old, as well as his thoughts on his right to die with dignity in South Africa. He noted that in contemplating ending his own life he had been surprised at the extent of the moral and practical support he had received.
Schoeman concludes the letter with, “My own impression is that this is an apt time to widely and openly discuss in South Africa the question of self delivery. Should I succeed in my current attempt, those involved are, as far as I am concerned, totally free to discuss this with the outside world. I hope that my death will contribute to a more general discussion than currently exists of the real problems of ageing as well as the question of self delivery. I also hope that it will help to amend current South African law with regard to self delivery. This is enough.”
In his farewell, Schoeman dispassionately writes that the decision to end one’s life was a “highly personal” issue that he would not “blindly” recommend. He explains that current South African law made provision for a Living Will which directed medical personnel not to intervene in a life-threatening situation. Another method of ending his life, wrote Schoeman, would be to fast – declining food and water – and in so doing starve to death.
“This is the method that I, in the absence of a dignified alternative, originally settled on for myself. It is a protracted way of dying and not necessarily without discomfort and pain, apart from the burden it places on those who are prepared to offer support during the process. Yet this is at least a dignified way to end life, which cannot be said for the alternative methods that are available in the current circumstances in South Africa.”
The writer, who was single – although the Afrikaans description “alleenlopened” (walking alone) is much more apt – begins his letter by expressing his wish not to grow old and revealing that he had decided years ago “to end my life, or at least try and end my life, timeously”.
He reveals that an attempt to end his life at the age of 75 had failed and says, “I am 77 and it has become necessary now to tackle this task while I still have mobility, physical freedom and the mental clarity to make a meaningful decision in this regard and to execute it effectively.”
He adds that he had become aware over the past two years that the research and writing that had kept him occupied for so long had become a burden and that he had “with a certain amount of relief” begun to distance himself from this. During this process, says Schoeman, he had grown acutely aware of his physical and spiritual decline.
“What lies ahead for me, in terms of my humanity, and in all likelihood, is an increasing condition of helplessness and dependence during which I will become a burden to myself and others.”
It is not exactly clear how Schoeman died – whether he did in fact opt to starve himself to death – or elected to use another method. An autopsy is still due to be performed.
Schoeman’s death and his plea for the debate about death with dignity comes at a time when Dignity SA is gearing up to continue to challenge legislation in South Africa with regard to assisted suicide and the right to die with dignity.
In December 2016 the Supreme Court of Appeal overturned a 2015 High Court Ruling granting the terminally ill lawyer, Robin Stransham-Ford, the right to die with dignity by way of euthanasia. The overturning of the ruling upholds the country’s current laws rendering assisted suicide a criminal offence.
Stransham-Ford, who had cancer, died a few hours before the High Court ruling and the SCA ruled that the claim ceased to exist once Stransham-Ford had died before the order could be granted, the Department of Justice has maintained. The ministry added that the SCA had held that this had been an inappropriate case in which to develop “the common law of murder and culpable homicide”.
Professor Sean Davison, chair of DignitySA, has continued to lobby for the amendment of South African law with regard to the right to die with dignity. In 2015 Davison posted on Facebook that he had spoken at a medical symposium in Cape Town attended by over 100 medical doctors.
“The title of my presentation was ‘The right to die with dignity’. I was expecting a cool response from the audience since it is a pattern throughout the world that doctors are reticent on the subject of assisted dying. To my surprise, when I polled the audience, 80% were in favour of changing the law to allow for assisted dying for the terminally ill. However, even more surprising, after I had presented my talk, was that at least 50% of the doctors supported assisted dying for those with ‘unbearable suffering’. Having doctors supporting our campaign for a law change is crucial to its success – I am now confident that we can get them on board throughout the country.”
Schoeman provided through his fiction some of these existential issues that he himself finally had to face and which he hoped would contribute to a more urgent endeavour to provide those who wish to do so the right to end their life with dignity.
His legacy exists not only in the fiction or grand historical accounts he wrote, but also in the reanimation of individuals, both well-known and obscure, whose forgotten lives he encountered in the archives and who he thrust back into public view. Schoeman is one of the country’s most important historians whose work exhorts us to take heed of the past.
“The past is another country; where is the road leading there?” writes Schoeman in one of his early novels, This Life.
He will most certainly be remembered for his parting gift, that of prompting us to engage with urgency the universal matter of the right to die with dignity. DM
Original Photo: Karel Schoeman (Netwerk24)

More than 140 applications to die have been made by terminally ill Victorians since voluntary assisted dying laws came into force on June 19. Figures seen by The Age show there have been about five applications a week in the first six months of the landmark euthanasia laws, with the scheme looking poised to far surpass preliminary estimates for the first year.

While the actual number of people who have died using the new laws is not yet known, it is estimated at least a dozen people have taken their own lives using government-endorsed medication. A person can make more than one application if they are initially rejected.
Eleven people received approval to end their lives within the first 11 days of the scheme's operation.
How Victoria's assisted dying laws work
Based on international experience, the state government predicted the number of patients accessing the laws could be as low as 12 in the first year, before stabilising at about 150 people a year.
Figures seen by The Age do not take into account how many permits have been granted, how many applications have been rejected, nor how many people have died using the medication provided under the new laws.
The state government would not comment on the data viewed by The Age, in keeping with Health Minister Jenny Mikakos' determination not to offer a "running commentary" on the progress of assisted dying.
The Voluntary Assisted Dying Review Board, which assesses every application, will release its next report in February which will reveal the number of people who have taken their own life using the laws.
Under the laws, two doctors, including an expert in the person's disease, must conduct favourable assessments of a person's eligibility. Doctors have the right to object to taking part in the scheme.
A person has to make three separate requests to end their life after initiating the process themselves.

Melbourne oncologist Cameron McLaren, who sits on the Dying with Dignity board, has helped 24 patients get permits.
The most profound-red tape hurdle for many of them, he said, was finding a specialist doctor in their disease who had undertaken the mandatory assisted dying training.

Dr McLaren often spends hours each week driving across the state to visit people wanting to end their lives. Most require up to three appointments even though many are bedridden or too ill to leave their homes.
Dr McLaren said there was a significant shortage of haematologists who had undertaken the training and were able to assess patients dying from blood cancer.
"As it currently stands, it's being upheld by very few of us," Dr McLaren said.
"The people involved in the scheme are doing a fantastic job but there is a real need for more specialist doctors to sign up.
"They need to realise they are not going to jeopardise their business or be tarred and feathered in the main street of Melbourne.
"They can provide a very valuable and compassionate service which gives people control of their bodies in the final days of their life.”
The laws allow access to a lethal substance for terminally ill adults who have only about six months to live – or no longer than 12 months for those with a neurodegenerative diagnosis – and who meet other strict eligibility criteria such as being able to give informed consent.
Most people will drink the dose – a lethal powder mixed with about 100 millilitres of a liquid medication – in their own homes at a time of their choosing.
Under certain circumstances, those too ill and physically incapable of swallowing will be allowed to take the substance through an intravenous drip set up by a doctor.
A spokeswoman for Ms Mikakos said the numbers of doctors registered with the assisted dying scheme had increased threefold since the laws came into effect.

“We are pleased with the number of doctors trained – and the increase in numbers is consistent with our expectations before the start of the laws," she said.
“We expect training numbers to continue to increase over time as doctors see the system in practice and more patients approach them."
The government declined to provide a breakdown of specialists but did reveal that 360 doctors have registered or completed the training including GPs, cancer specialists and palliative care clinicians. About a third of doctors are based in regional Victoria.
The government stressed there were processes in place for those struggling to find a doctor who had undertaken the training, including three voluntary assisted dying care "navigators" who are based at the Peter MacCallum Cancer Centre, providing patients, doctors, and hospitals across the state with information and support.

LINKS



Red Jos: HUMAN RIGHTS ACTIVISM
Mannie and Kendall Present: LESBIAN AND GAY SOLIDARITY ACTIVISMS
Mannie's weblogs may be accessed directly by clicking on to the following links
Activist Kicks Backs - Blognow archive re-housed - 2005-2009
RED JOS BLOGSPOT (From January 2009 onwards)

This page created on 29 SEPTEMBER 2016 and updated on 10 JANUARY 2020
PAGE 88